Watching the health workers in China, I always doubt that they could work in their protective attire efficiently for a long time. They looked more like intimidating alliance from a space ship. What are their boots for? As I can see on the TV, people, who are working in the patients wards in USA, are ”packed” in Personal Protective Equipment (PPE), which does not contribute to efficient work.
Is SARS-CoV-2 different from other previously known Corona viruses? As far as we know from the open press, this virus is not different except more transmittable and contagious, which is still questionable, and unfortunately more excessive morbity and obviously mortality, like in Italy. The Italy’s case still is waiting for sober analysis.
As far as Personal Protective Equipment (PPE) is concerned, Occupational Safety and Health Administration (OSHA) in Guidance on Preparing Workplace for COVID-19 states: ”Workers, including those who work within 6 feet of patients known to be, or suspected of being, infected with SARS-CoV-2 and those performing aerosol-generating procedures, need to use respirators.”
The most popular is NIOSH-approved fit-tested N95. On the paper this looks easy. OSHA recommends the employer, the employer requires the employee, but it is extremely difficult to work by using a N95 respirator for a prolonged time.
No any anatomic pathology laboratory work meets the of mentioned above requirement as well as “close contact” situation. The weak place is the frozen section procedure which requires a separate presentation.
Center of Disease Control and Prevention (CDC) defines “close contact” as being about six (6) feet (approximately two (2) meters) from an infected person or within the room or care area of an infected patient for a prolonged period while not wearing recommended PPE. Close contact also includes instances where there is direct contact with infectious secretions while not wearing recommended PPE. Close contact generally does not include brief interactions, such as walking past a person.
CDC does NOT currently recommend the general public use facemasks.
When I see medical personnel in an Italian patient’s ward, my feeling is that they cannot provide an effective care in such attire despite ventilators and best in the world medication. They require special personnel to dress and undress them. They are living people who have physiological needs. In my understanding, such PPE can be used for a short time during procedures which include placing or removing from a ventilator, suctioning air ways, bronchial lavage, etc.
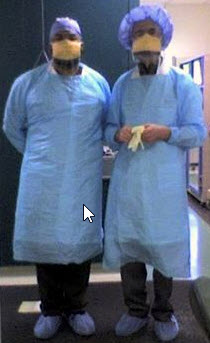
In the complete adherence to OSHA for COVID-19 recommendations, a workable attire should include following items: a disposable plastic gown (tied on the back), cap (covering ears completely), goggles type glasses, a protection mask with a shield, and disposable gloves. In my view, doble glows are obligatory (explanation later). This is not a cavalierly rather a realistic approach.
For many years, I used the Upsidedown Kimberly-Clark FLUIDSHIELD mask on a regular basis during my work in the surgical pathology grossing room. (See more details The Protection Masks post).
The main crucial point of using PPE is how the attire is taken off. In this regard, some considerations of the ways for infection transmission would be appropriate to present. This knowledge would be useful for the general public as well.
The SARS-CoV-2 virus, if it exists in given environment from any source, dwells in wet surroundings, more or less size droplets from their human carriers (ill or not). The virus does not jump, but semi-dried out attached to the protective attire (otherwise why the attire is used), the virus can reach the “entrance gates” (medical term) for infection (nose, mouth, eyes) just at the moment when the attire is taken off. This brings us to the rational mode how to take off PPE.
On the TV, I’ve seen how a doctor took off his protective gown and gloves with fast movements while placing them into an open large bucket. This is dangerous for him and the environment, especially in the limited room space under air conditioning circulation.
There are certain common-sense rules which I have inherited during my training and work as an epidemiologist.
First, the take off the attire should be in slow motion manner.
Second. Following a certain sequence of taken off items: with still gloves on, the gown is taken off the first; it is slowly folded with external side inside and rolled before place in the collection bucket; then the double glow is taken off; then the cap is taken off in the same manner; then protection of eyes/face with gloves off. The internal gloves are taken off slowly, rolling the glove from one hand and taken off from the second hand using the rolled glove as a tool. Both rolled gloves are slowly placed in the trash bucket.
Hand wash and all open face’s hair areas (eyebrows, mustache, beard) by closed eyes.
The presented PPE principles are applicable in private life. Understanding of the rationale of infection protection can be helpful in different everyday life situations. The angel is in understanding of the details.

