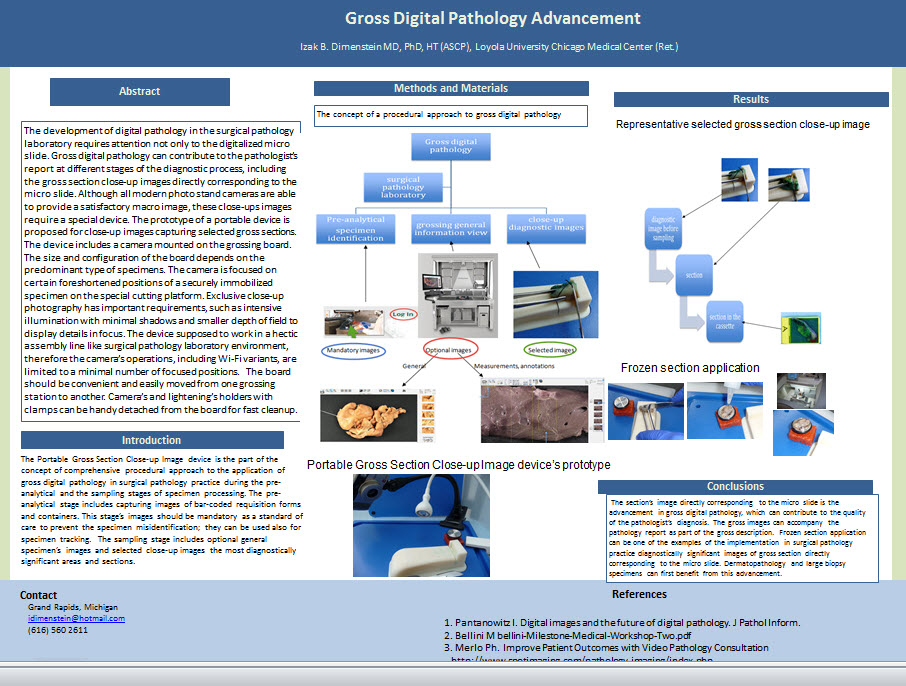
The frozen section laboratory has the highest level of potential infection exposure in surgical pathology. The specimen in a fresh state is processed in a justifiably rushed pace. By the nature of trimming/cutting, multiple micron size fragments are generated in aerosol form in the cryostat. It is the common understanding that cryostat’s chamber accumulates potentially dangerous infectious materials for the worker as well for other people in the room. Hopefully, time has gone when cryostats were full of remnants of trimmed and cut tissues of previous frozen sections cases. As a matter of common sense, cleaning of the cryostat’s chamber is everyday routine in most laboratories though is not regulated yet. The cryostat’s defrost cycle continues the cleaning job.
The official CAP Laboratory Accreditation Program check list (ANP. 12807 Phase II revised 06/15/2009) states: Is there a documented procedure for the routine decontamination of the cryostat at defined intervals, and are decontamination records evident? NOTE: The cryostat must be defrosted and decontaminated with a tuberculocidal disinfectant at an interval appropriate for the institution; this must be weekly for instruments used daily. Trimmings and sections of tissue that accumulate inside the cryostat must be removed during decontamination. Although not a requirement, steel mesh gloves should be worn when changing knife blades.
The regulations also state that the cryostat must be clearly marked as contaminated if a frozen section is performed on tissue from a patient known or suspected to be positive for HIV, hepatitis B or C, SARS-related coronavirus, prion disease such as Creutzfeldt-Jakob disease, mycobacterial or systemic fungal disease. It must then be decontaminated before further use.
There are mycobacterial reagents which could be used in suspicion or certain tuberculosis infection (tuberculocidal disinfectants). For example, PD-128 by Spartan Chemical (http://www.spartanchemical.com/products/product/101604)
CaviCide ( Metrex http://www.metrex.com/) looks as too expensive for the cryostat’s chamber cleaning, but this is my own opinion.
Some laboratories use a weekly schedule (for the daily use cryostats it is obligatory by CAP requirements), some monthly, nobody, I guess, uses steel mesh gloves when changing the blade, but the main thing is to do decontamination diligently and correctly. The method of the cryostat’s chamber cleaning are very much standard. The bottom line is that decontamination, the process of removing foreign material such as blood and body fluids, does not completely eliminate microorganisms. But it is a necessary step preceding disinfection.
Here is a possible method of scheduled cryostat chamber’s decontamination and disinfection.
The details of cryostat maintenance are presented at http://www.histologytutorials.com/ website. This is an excellent practical guide.
There is also an excellent systematic instruction on cryostat decontamination by Leica Microsystems (see in the end of this article.)
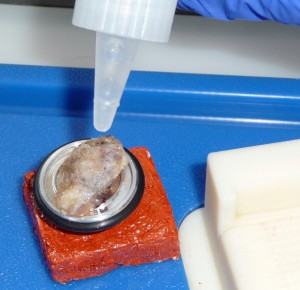
The work starts after the cryostat is plugged out and the chamber reaches room temperature. Everything removable is taken out, including a blade from the holder for separate cleaning. The debris is taken carefully mechanically out by using a brush with a long handle, like Leika’s microtomy brush. Debris must be removed as much as possible because it may hinder the chemical disinfectant access to contaminated surfaces. Sponges with 70% ethyl alcohol should be used to clean the cryostat’s chamber. (Alcohol is most effective in the 70% range because it can penetrate better than absolute alcohol. Absolute alcohol creates a protein coagulation film. It can be used only after 70% alcohol as a final step, as well as to take out moisture, but not before defrost and other cleaning procedures).
Absorbent disposable towels with disinfectants, for example CaviWipes http://www.metrex.com/ , are placed (not sprayed to prevent creation of aerosols!)onto surfaces of the chamber allowing them to remain in contact with contaminated surfaces for the length of time specified in the instructions of the individual agents. After the disinfection procedure is complete, the cryostat and all of the accessories must be thoroughly dried (Absolute ethyl alcohol can be used to remove excess moisture from surfaces). Just a practical remainder to lightly lubricate any moving parts before being put back into service at cold temperatures because difficulties in cutting during frozen sections create necessity of additional trimming that increases debris.
All cleaning materials should be treated as biohazardous waste and disposed according to the institution’s policies and procedures. The liquid waste container also should be emptied.
There might be different protocols. For example, models which have the heating block filled with 40% formaldehyde during the overnight decontamination cycle. After this process, the debris is removed using paper tissue damped with 70% ethanol.
There is a protocol of fuming the chamber for 24 -48 hours with formalin with following neutralization with ammonia. This method is cumbersome. The cryostat is out of work for two days. Its practicality is questionable.
The same procedures are carried out immediately after a case was finished if anything suspected of being an infective agent had been cut. If the cryostat’s use for the next frozen section were expected, a regular cryostat need 3 hours to reach a proper cooling temperaturefor optimum sectioning. Every laboratory that practices frozen section should have at least three cryostats with one of them designated for known or suspected curtain infectious material, e.g. tuberculosis, AIDS, Methicillin-resistant Staphylococcus aureus (MRSA), etc. Additional to three amounts of cryostats depends on the work load.
Cryostat manufacturers offer some models which assure disinfection of the chamber. Although there are no studies in literature of their effectives and reliability, besides manufacturer’s statements, this is a positive tendency. For example, The Leica’s CM1850 UV 9 is equipped the cryochamber with ultra-violet light (UVC) for disinfection. Vibratome UltraPro 7500 Self-Decontaminating Cryostat offers a spray-jet liquid decontamination (a solution which includes peracetic acid and hydrogen peroxide.) Decontamination requires 3.5 hours. UV radiation is successfully used in the destruction of airborne microorganisms, but UV light sterilizing capabilities are limited on surfaces because of its lack of penetrating power.
Mutually condemned, the most dangerous is the use of freezing sprays. A cloud of aerosol particles surrounds the person bend to microtome in the cryostat’s chamber. They can be inhaled or even reach eyes. Although some tricks can be made as spraying the chuck outside the cryostat’s chamber, this method is used rarely in practice due to time and quality of section considerations. In general, it is unwise to use propellant under regular freezing conditions; especially the modern cryostats provide technical solutions like built-in-Peltier units or cold metal bars that can cool specimens fast. Variants of instant deep freezing, like in liquid nitrogen can be used.
There are some official documents in this regard.
Federal Registry 1910.1030: “All procedures involving blood or
other potential infectious materials shall be performed in such a manner
as to minimize splashing, spraying, spattering, or generation of droplets
of these substances.”
NCCLS (now CLSI) Document M29-T: “Frozen sections done on unfixed
tissue pose a high risk because accidents are common. Freezing of tissue
does not inactivate infectious agents. Freezing propellants under
pressure should not be used for frozen sections as they may cause
spattering of droplets of infectious material.”
Improvements in quality of cryostat’s freezing can diminish the use of sprays, but the problem exists of section warming during the cutting that leads to uneven and thicker than desired sections. Or, in some occasions, for example, the specimen falls out from the chuck during the cut. Sometimes is necessary to change the position on the chuck and to continue sectioning immediately. Many unforeseen situations occur during the hassle of frozen section. If the spray were used for some reasons, it is necessary to clearly understand the danger.
Gradually the requirement of wearing a mask becomes more and more implemented. But what kind of a mask is appropriate for frozen section unit? OSHA does not determine kind of mask specifically for the frozen section laboratory. The question of protective mask will be discussed separately.
The second problem related to infection exposure in frozen section unit is a finger cut by the blade. Nobody can work in metal mesh gloves. Although the section usually (with many exceptions) is taken off with a brush, cuttings do occur by some hardly predictable circumstances. With experience they occur rarely. The injured ought not to continue to work, as often takes place. Every occurrence of finger cut should be handled like needle stick injury according to the institution’s protocol.
Some references:
National Committee for Clinical Laboratory Standards (NCCLS), Protection of laboratory Workers from Instrument Biohazards and Infectious Disease Transmitted by Blood, Body Fluid and Tissue; Approved Guideline M29-A, Wayne, PA, NCCLS 1997.
Frozen Section Technique for Tissues Infected by the AIDS Virus,
Swisher, B.L., Ewing, E.P., J Histotechnology, V9, No.1, p.29 (March 1986)
APIC Guideline for Selection and Use of Disinfectants, Association for
Professionals in Infection Control (APIC), American Journal of Infection
Control, Vol 24(4), August 1996, 313-342.
Leica 1950 (http://www.leicabiosystems.com/specimen-preparation/sectioning/cryosectioning/details/product/leica-cm1950/) is not only in my experience the excellent working horse in the surgical pathology frozen section laboratory, but also is very convenient for reliable decontamination and disinfection. Below is the official Leica’s instruction.
Leica Microsystems cryostat decontamination instruction by Jan Minshew
Chemical Disinfection of a Cryostat
According to CAP regulations, a cryostat should be defrosted and decontaminated with a tuberculocidal disinfectant at a time interval appropriate for the institution (once a week for instruments used daily). The regulations also state that the cryostat must be clearly marked as contaminated if a frozen section is performed on tissue from a patient known or suspected to be positive for HIV, hepatitis B or C, SARS-related coronavirus, prion disease such as Creutzfeldt-Jakob disease, or mycobacterial or systemic fungal disease. It must then be decontaminated before further use.
Wear Personal Protective Equipment (PPE):
Personal Protective Equipment, such as gowns, puncture and penetration resistant gloves and eye protection must be worn when performing cryostat disinfection procedures.
Cryostat Preparation
Remove used blades/knives from their holder. Although not a requirement, steel mesh gloves should be worn when changing knife blades. Dispose of blades according to the regulations of the institution or disinfect knives before reusing by soaking in disinfecting solution. Remove all debris and utensils (pencils, forceps, brushes, gauze, etc) from the chamber. Debris must be removed because organic material (blood and proteins) may contain high concentrations of microorganisms and could possibly inactivate the chemical disinfectant or prevent access to contaminated surfaces. It should be treated as biohazardous waste and disposed of according to the policies and procedures of the institution. 70% ethyl or reagent alcohol can be used to clean the cryostat and provide some disinfection capabilities. The germicidal activity of ethyl alcohol is most effective in the 70% range because it can penetrate tubercle bacteria and it has an advantage over isopropyl alcohol of being able to kill hydrophilic viruses.
Chemical Disinfection
In order to disinfect a cryostat using a chemical disinfectant, the instrument MUST be at room temperature before the process is started. Turn off and unplug the instrument before beginning the disinfection process. (Once the cryostat has reached room temperature, do not turn the handwheel until it has been returned to cold temperature.)
Chemical Disinfection of a Cryostat continued:
Do not create aerosols by spraying disinfectant (or anything else) in an open cryostat chamber. Pour disinfectants onto surfaces or absorbent disposable towels and allow them to remain in contact with contaminated surfaces for the length of time specified in the instructions of the individual agents. Use a tuberculocidal disinfectant that is non-corrosive. The EPA maintains a list of Antimicrobial Chemical/ Registration Number Indexes on their website, http://www.epa.gov/oppad001/chemregindex.htm), and it is updated regularly. From this link you can find agents effective against bloodborne pathogens such as Mycobacterium tuberculosis, human HIV-1 virus, and Hepatitis B or Hepatitis C virus. It is critical to remember that NONE of these solutions have been tested at low temperatures and can only be used at room temperature. Any disposable material used in the disinfection process must be disposed of in accordance with the policies and procedures of the institution.
Following Disinfection
After the disinfection procedure is complete, the cryostat and all of the accessories must be thoroughly dried and lubricated before being put back into service at cold temperatures. Absolute ethyl alcohol can be used to remove excess moisture from surfaces. Accessories with multiple parts, such as the disposable blade holder, knife holder and their respective bases, must be taken apart and dried thoroughly.
Plug the instrument back in and turn it on. Use only the lubricants that are recommended by the manufacturer and only in the recommended amounts. Lightly lubricate any moving parts. To lubricate the specimen arm, extend it all the way forward. Apply ONE DROP of lubricant to the barrel and spread it around with your gloved finger. Move the arm back to the home position.
The liquid waste container should be emptied in accordance with the policies and procedures of the institution. Before replacing in the instrument, add a small amount of liquid bleach to the empty container. For optimum sectioning, allow the instrument to cool long enough to allow the metal microtome parts to reach the cold temperature setting. The CM1850 requires no less than 3 hours and the CM1950 needs 5 hours to cool down from ambient temperature (20°C) to -25°C and 8 hours to cool from 20°C to -35°C.
See also in the post Ebola Highlights Work Space Safety